IVF FAQ
- How is female reproductive anatomy involved in the conception of a baby?
- How do the menstrual cycle and hormones impact ovulation?
- What are the benefits of IVF?
- What procedure is right for me?
- How do we determine what type of cycle I will have?
- What is the difference between a birth control versus no pill cycle?
- What is a protocol? How does my provider determine the approach?
- Are there risks with IVF?
- How do I prepare for fertility treatment?
- How long should I plan to be at the clinic on my procedure date?
- How many embryos do you transfer?
- What are the concerns surrounding having twins?
- What are the risks/side effects?
- What should I expect during recovery?
- How do I find a support group/counseling outside of friends and family?
- Are there egg/sperm/embryo storage facilities at the KP Centers for Reproductive Health?
If you are considering in vitro fertilization (IVF), it’s understandable to have a lot of questions. The following information can help you understand the how and why of the treatment process.
How is female reproductive anatomy involved in the conception of a baby?
Eggs develop, are stored, and mature in the ovaries. The fallopian tubes pick up the eggs (usually 1 per month) that are released from the ovary during ovulation. The sperm is deposited into the vagina during intercourse. Because the sperm are generally motile, they enter the cervix and uterus and travel into the fallopian tubes to fertilize an egg. If an egg is fertilized, an embryo is created. The embryo will travel down the fallopian tube to the uterus to implant. This occurs about 5 days after the egg and sperm join to create the embryo. The uterus has a specialized lining called the endometrium that allows an embryo to implant into the wall providing the developing baby with nutrients and support.
How do the menstrual cycle and hormones impact ovulation?
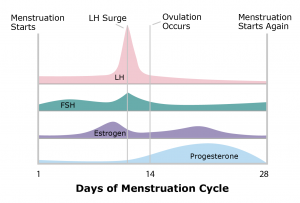
The entire menstrual cycle is controlled by the brain in concert with the ovaries. There are 5 main hormones involved in reproduction.
The following 3 are produced by the pituitary gland in the brain:
- Follicle stimulating hormone (FSH) stimulates the growth of the egg within the ovary.
- Luteinizing hormone (LH) stimulates ovulation for the release of the egg.
- Prolactin stimulates milk production.
Estrogen and progesterone, produced in the ovaries, help prepare the lining of the uterus for a fertilized egg.
The menstrual cycle is measured in days, where day 1 is the first day of the menstrual period. Ovulation usually occurs at approximately day 14. If the released egg is not fertilized, the lining of the uterus (the endometrium) is sloughed off as the menstrual period. Although a 28-day cycle is shown in the illustration, most women’s cycles vary in length.
What are the benefits of IVF?
IVF services can be personalized to fit the needs of the patient and can have a higher success rate when other treatments are not successful.
IVF treatments can help decrease the probability of miscarriage. Genetic abnormalities are the most common reason many women have miscarriages. With the advancement of pre-implantation genetic testing (PGT), we are able to test individual embryos and can transfer those without genetic abnormalities. Prenatal genetic testing during pregnancy is still encouraged to confirm the genetic testing results.
Unlike natural fertilization, IVF does not involve the woman’s fallopian tubes, so if these are blocked, damaged or absent, pregnancy is still possible.
Additionally, IVF treatments may be an option for those experiencing Male factor infertility.
What procedure is right for me?
Your procedure will be dependent on the results of your tests, lifestyle, and other factors discussed with your provider. Your provider will then determine the right protocol for you.
How do we determine what type of cycle I will have?
Multiple factors are considered when determining the most effective approach to ovarian stimulation and the type of cycle. Your ovarian reserve, as determined by hormone levels and antral follicle count (“egg count”) will be an important factor in this decision. Stimulation medications will begin within a few days of the start of your period.
Your medical history may be used to determine what protocol is best for you. Your provider will discuss your medical history in depth to determine what protocol is best for you.
What is the difference between a birth control versus no pill cycle?
During your normal monthly menstrual cycle, multiple follicles (tiny sacs in the ovaries where eggs mature) will begin to grow, but only one will continue growth and become dominant. The goal of ovarian stimulation medications is to have multiple follicles continue to grow at the same rate, thus increasing the number of mature eggs collected during the egg retrieval. The use of birth control pills in the beginning of the cycle provides several benefits, which include:
- Helping the follicles grow at the same rate.
- Preventing ovarian cysts from developing and possibly interfering with the cycle.
- Enabling the clinic to schedule egg retrieval.
- Allowing the patient to plan for time off work, vacations, etc.
- Helping the laboratory and embryologists schedule staff and incubator space.
What is a protocol? How does my provider determine the approach?
A protocol is a treatment plan developed by your provider that includes your specific medications and procedure plans for the type of cycle you are planning to pursue.
- Think of a protocol as the guideline for:
- Medications and the doses you will be using.
- The plan for fertilizing collected eggs.
- Additional embryo testing (as needed).
- The type of embryo transfer you plan to have.
This information is also communicated to our IVF case managers (nurses) who will guide you through the process.
Are there risks with IVF?
As with all medical treatments, some risks exist. For example, a small percentage of women may experience ovarian hyperstimulation caused by the hormones used to prepare for IVF. The symptoms can range from mild to severe. Your provider will counsel you on these risks and how they will be managed during your cycle.
Multiple births are also possible with IVF. The Kaiser Permanente Centers for Reproductive Health follow the American Society for Reproductive Medicine (ASRM) and the Society for Assisted Reproductive Technology (SART) recommendations for embryo transfer, which have led to an increase in single embryo transfers and a decrease in the likelihood of multiple pregnancies.
How do I prepare for fertility treatment?
During your IVF consultation, your provider will discuss the need to be on pre-natal vitamins and other supplements. Preparing for your actual day of treatment begins when you start your cycle. Medications are used in many different cycles and are specific to your treatment plan. Some women may begin medications around ovulation to prepare for stimulation, while other cycles do not begin medications until their period begins. Your fertility treatment plan will be reviewed with your provider during your consultation. You will be given specific instructions by our nursing team that will address any questions you may have about medications, injections, cycle timing, and consent forms.
How long should I plan to be at the clinic on my procedure date?
This varies with each procedure, as follows:
- Egg retrieval: plan to be in the clinic for about 2 to 2.5 hours total.
- Embryo transfer: plan to be in the clinic for at least an hour.
You will be required to have a responsible individual accompany you when leaving the clinic. You will not be allowed to drive or leave unaccompanied. This is due to the nature of the sedation for the procedure, and for your own safety. Medications used for these procedures can cause drowsiness, fatigue, and lightheadedness.
How many embryos do you transfer?
The Northern California Kaiser Permanente Centers for Reproductive Health follow the guidelines set forth by the American Society for Reproductive Medicine (ASRM) and the Society for Assisted Reproductive Technology (SART) when determining the appropriate number of embryos to transfer. These guidelines are based on several factors including age, embryo stage, and embryo quality. Your IVF provider will discuss with you the number of embryos recommended for your transfer.
What are the concerns surrounding having twins?
Although the prospect of conceiving twins may be attractive for some people, the potential risk of complications for mother or babies during a twin pregnancy is higher than with a singleton pregnancy. Multiple pregnancies may increase the risk of miscarriage, premature births and other medical problems for mother and/or babies.
What are the risks/side effects?
Injectable medications may cause mild side effects. These include headaches, bloating, constipation, breast tenderness, fatigue or irritability. Bruising or swelling at the injection sites are also common. If you are experiencing any of these, or other side effects that are not listed, please contact one of the IVF case managers for further discussion.
IVF treatments are relatively low-risk procedures for most patients. In patients with a history of medical problems, your provider will discuss specific measures that can be taken to lower your risks during IVF treatment.
What should I expect during recovery?
After an egg retrieval, you can have soreness in the lower part of your abdomen. This will feel like menstrual cramps. Spotting after an egg retrieval can be normal. You may also feel bloated with mild tenderness in the pelvic area. These symptoms usually subside within a few days. Should you begin to experience more symptoms, such as increasing abdominal pain, period-like bleeding, fever, difficulty with urination or shortness of breath, contact the clinic for further evaluation or, if you feel that you are experiencing a life-threatening emergency, please call 911 or go to the nearest emergency room.
How do I find a support group/counseling outside of friends and family?
There are many resources and supporting communities for those in any stage of treatment. These communities are available both online and in person. Speak with your provider, nurse, or clinical team to identify the best resources based on your needs.
Are there egg/sperm/embryo storage facilities at KP?
Before your procedure, you will review and sign agreements that allow temporary short-term courtesy tissue storage at Kaiser Permanente. Following this short-term period, the tissue (e.g., sperm, egg, embryo) will be shipped for long-term tissue storage at our designated third-party facility, where you will be responsible for ongoing storage fees, unless insurance benefits apply.
Courtesy storage only applies to samples kept at Kaiser Permanente for the first 6 months of storage. Certain cases require that tissue be sent to our third-party storage facility immediately. In these cases, short-term courtesy storage does not apply, and patients are responsible for storage fees in these cases.
Please speak to a member of the IVF care team about any questions or concerns not addressed here.
Source: The Art of Conception, Kaiser Permanente, The Permanente Medical Group
Source: Reproductive Endocrinology and Infertility Department, The Permanente Medical Group
